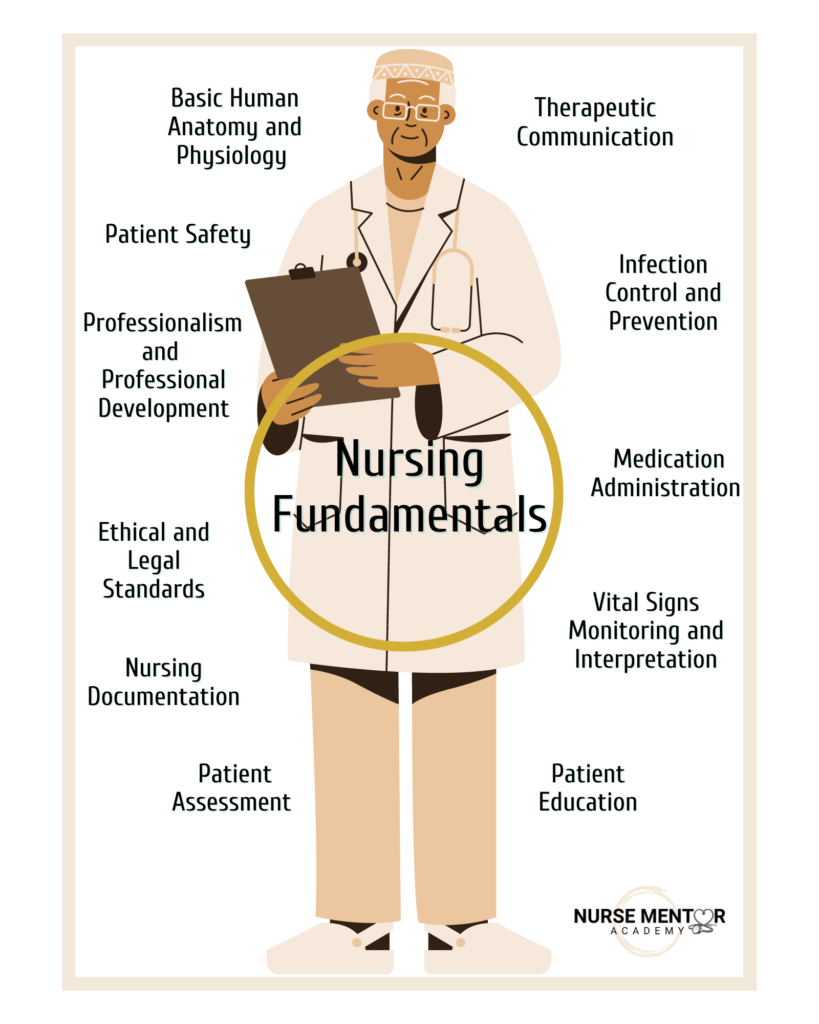
As an experienced nurse, I understand the importance of nursing fundamentals in shaping a nurse’s education and the future of nursing practice. These key components are the building blocks for safe and effective patient care. In this article, I will guide you through 11 essential elements of nursing fundamentals, sharing insights and personal stories to help you fully grasp these concepts.
Nursing Fundamentals: Understanding Basic Human Anatomy and Physiology
Understanding human anatomy and physiology is vital for nurses. It forms the core of our ability to assess and interpret physiological changes in our patients. Imagine my early days as a nursing student grappling with the complexities of the circulatory system. I vividly recall the moment when it all clicked – the heart’s role in pumping oxygen-rich blood throughout the body, the intricate network of blood vessels, and the importance of blood composition. This knowledge allows nurses to identify abnormalities and plan appropriate nursing interventions.
The Circulatory System: A Lifeline for Patient Well-being
For example, the circulatory system, comprising the heart, blood vessels, and blood, is the center of human anatomy and physiology. Understanding how the heart functions enables nurses to assess vital signs accurately and recognize signs of deficient perfusion. This means that the heart is not working correctly, and the patient is most likely not having enough oxygen circulating in the body. I recall a newborn who presented with a weak and thready pulse, accompanied by pale and cool extremities. This nursing assessment prompted immediate action, as it indicated poor perfusion and potential cardiovascular compromise.
I initiated protocols to assess the newborn and put him on oxygen while waiting for the team. By understanding the circulatory system, the nurse can intervene quickly to address these critical issues and, in return, promote the best patient outcomes. Therefore, nursing students need to understand the concepts taught in the human anatomy and physiology classes because this knowledge will be applied when caring for their patients as a fundamental nursing skill.
Therapeutic Communication
Effective communication is the core of nursing practice because it helps establish meaningful connections (rapport) with the patient and family. It is best to ask open-ended questions to learn more about the patient, such as “Tell me more…” As a nursing student, I discovered the transformative power of therapeutic communication. We create an environment where patients feel heard, understood, and supported through active listening, empathy, and clear expression.
One memorable interaction involved a patient expressing fear and anxiety about an emergency cesarean birth. Her birth plan included the necessary steps for a natural delivery, but the baby was not tolerating the labor, and the baby’s heart rate repeatedly kept dropping. I held her hands while explaining the procedure of cesarean birth, listened to her concerns, answered her questions, and assured her that I was going to be with her throughout the entire process while the team was pushing her bed to the operating room. By actively listening, showing empathy, and acknowledging her concerns, I was able to provide emotional support and alleviate her anxiety. This story exemplifies therapeutic communication’s profound impact on patient’s well-being. Remember that nurses have the fantastic power to be your patient’s advocate.
Infection Control and Prevention
Infection control is paramount in healthcare settings to prevent the spread of infectious diseases. Given the experiences learned from the COVID-19 pandemic, hand washing and wearing a facial mask became the new normal for many people. As a nursing student, I learned the importance of adhering to standard precautions, such as proper hand hygiene, appropriate use of personal protective equipment (PPE), and meticulous handling of contaminated materials. I recall an incident where a patient was diagnosed with a highly contagious respiratory infection. By donning appropriate PPE and following strict infection control protocols, we effectively contained the spread of the infection, protecting both patients and healthcare providers. This practice is common in many medical-surgical hospital units, and nurses must be proactive to prevent the spread of infection.
Medication Administration
Safe and accurate medication administration is a critical responsibility of nurses. As a nursing student, I remember the meticulousness required when administering medications. Nursing students must pass a medication calculation test before they are allowed to administer medication under supervision during clinical rotations. Understanding the “Five Rights” – ensuring the right patient receives the right medication, in the right dose, through the right route, and at the right time – is crucial.
I recall a patient who had multiple medications prescribed, each with unique dosing requirements. Through careful calculations and verification, I administered the medications accurately, minimizing the risk of adverse effects and promoting optimal patient outcomes. Some common medication errors include administering the wrong medication to the patient because of multiple medications with similar names or administering an unsafe dose of a medication. Medication barcoding systems used in many healthcare systems have checks in place to decrease medication errors since both the medication and the patient must be scanned before administration. Additionally, some healthcare institutions now require 3 patient identifiers at the bedside, including the patient’s full name, medical record number, and date of birth.
Patient Assessment
A head-to-toe patient assessment is a fundamental skill for any nurse. Nurses gather data about the patient’s physical, emotional, and psychosocial well-being through observation and effective interviewing techniques. Subjective data is the information the patient shared with you, such as their pain score of 7 out of 10, and objective data is the data you collect, like the blood pressure reading or temperature. I recall a patient who presented with a boggy (soft) uterus after giving birth, but through a comprehensive assessment, I identified subtle signs that led to the discovery of postpartum hemorrhage, which could be life-threatening. The patient was taken immediately to the operating room for treatment. This experience taught me the significance of thorough assessments and the power of keen observation in uncovering hidden clues. Nurses must always listen to their intuition which is a powerful underrated gift.
Patient Education
Nurses educate patients daily. It could be on how to self-administer an injection, what foods to not eat, exercises to complete, or signs and symptoms to report. Patient education could be verbal, where the nurse explains the information, or it could be demonstrated, where the nurse shows the patient how to complete a task. The use of patient-approved booklets, flyers, or videos could supplement patient education. As a newborn transition nurse, I educated new parents on every procedure I did for their babies.
I recall a couple adamant about their baby not receiving any medication and refusing the routine vitamin K injection. Despite some efforts to educate them on the risks and benefits of the medication, they still refused. I brought in an additional resource: a video showing the dangers of what could happen if a newborn started to bleed and did not receive the vitamin K injection. The video resonated with the parents, who immediately thanked me and agreed to administer the vitamin K injection to the newborn. The lesson here is that education is robust, and sometimes nurses need to have alternative options to get information across to patients.
Vital Signs Monitoring and Interpretation
Monitoring and interpreting vital signs are essential nursing skills. These parameters provide crucial information about a patient’s overall health status. The vital signs include temperature, pulse, blood pressure, and respiratory rate. The normal ranges for vital signs also differ based on the age group. For example, a respiratory rate of 16 is within normal limits for a healthy adult; however, critically too low for a newborn. The typical vital signs for a newborn, older child, and adult are different; nurses must have this knowledge based on the population they are caring for. Through meticulous measurement techniques and accurate interpretation, we can identify trends, monitor responses to interventions, and detect early signs of deterioration. I remember caring for a mom who recently delivered a baby, and her blood pressure dropped significantly, and her heart rate increased rapidly. This alerted me to a potential crisis, prompting swift action and the involvement of the healthcare team.
I immediately considered the potential of this new mom losing a significant amount of blood and vital signs. Monitoring helped to improve her condition, allowing the team to intervene promptly for an optimal outcome. Therefore, accurate measurement techniques and interpretation of vital signs for identifying patient status changes are critical nursing skills. For example, using the right size blood pressure cuff for a specific patient and placing the cuff in the right location is vital to get an accurate result. Understanding the patient’s age and position of the patient when the blood pressure was taken also plays a role in interpreting the results.
Nursing Documentation
Adequate nursing documentation and reporting are fundamental aspects of nursing practice. Nurses need to develop individual care plans to provide individualized patient care. Creating a nursing care plan involves assessment, goal setting, intervention selection, and evaluation. For example, if a patient is suffering from anxiety might be found to have an elevated heart rate during an assessment. A realistic and measurable goal would be for the patient’s heart rate to be between 70 and 100 by the end of the shift. A nursing intervention within the scope of practice might be implementing deep breathing exercises and meditation twice daily. By the end of the shift, the nurse would evaluate the effects of the intervention by assessing the patient’s heart rate to evaluate if the outcome was achieved.
As a nursing student, I quickly learned the importance of clear and comprehensive documentation. Accurate records ensure continuity of care and serve as a legal and ethical responsibility. As a nursing student, my instructors always said that if something was not documented, it was never done. This means that it does not matter how great care you provide to the patient because if you did not document that care, there is no proof that it was done. I recall an incident on my unit where thorough documentation by the previous shift nurse helped identify a potential medication error.
The nurse documented the detailed conversation she had with the family member at the bedside during admission about the patient’s home medications. This allowed the next shift’s nurse to compare the previous notes with the medication orders the healthcare provider placed, enabling the immediate correction of the situation. This situation also highlights the significance of documenting assessment findings accurately because this patient was never prescribed blood pressure medications at home; however, during admission to the hospital, she was hypertensive (her blood pressure was elevated). Adequate documentation promotes effective communication among healthcare providers, ensuring a holistic approach to patient care and safeguarding patient welfare.
Ethical and Legal Standards
According to the Gallup polls, nursing is among the most trusted and ethical professions. Ethical and legal considerations play a significant role in nursing practice. As future or current nurses, understanding ethical principles and legal obligations is crucial for navigating complex healthcare scenarios. Fundamental ethical principles such as autonomy, beneficence, nonmaleficence, and justice help nurses care for patients within ethical standards. Legal considerations such as informed consent, patient rights, and the nurse’s role in advocating for patient welfare help nurses provide safe nursing care.
I recall a challenging situation where patients’ autonomy clashed with their immediate health needs. This young mother lost a lot of blood during childbirth and was symptomatic with increased heart rate, dizziness, and fatigue. However, based on her religious beliefs, she refused any blood-based products, including a blood transfusion. Balancing respect for the patient’s autonomy while advocating for her well-being requires careful consideration of ethical principles. Initially, it was challenging, but knowing that my patient felt empowered and respected was most rewarding. Familiarizing yourself with ethical frameworks and legal standards empowers nurses to make informed decisions and deliver care that upholds patient rights and welfare.
Professionalism and Professional Development
Professionalism is the cornerstone of nursing practice. As nursing students, we must embody the qualities and attributes of professional nurses. Commitment, integrity, and a dedication to lifelong learning are hallmarks of professionalism. Nurses are continuously required to learn new things and maintain a level of competencies within their scope of practice. Continuing education hours are required for license renewal every two years. Nurses must also be culturally competent to provide patient-centered care. This means that nurses must understand and respect why people of different cultures engage in certain practices. I recall one of my nursing students removing a wrapped piece of thread from a Haitian baby’s forehead, thinking it was lint. I quickly explained to her that the thread was placed on the baby’s forehead to prevent any “evil eye” and keep the baby safe, a practice by many Caribbean families.
Also, many nurses are board-certified in different nursing specificities based on their practice interests. For example, about two years after becoming a nurse, I passed another exam to become board certified in maternal-newborn nursing. I also joined a national nursing organization within my specialty as a member, which later became a leadership position as a chapter leader for the local chapter in my county. I also returned to school to earn master’s and doctoral degrees, which opened endless opportunities for career growth. Nurses should find a mentor who continually exemplifies professional qualities and inspires them to seek opportunities for professional growth. You can foster personal and career growth by joining professional organizations, pursuing further education, and actively engaging in professional development. An experienced professional nurse ultimately has the potential to deliver the highest quality of care to patients.
Patient Safety
Patient safety and risk management are critical components of nursing practice. Through a proactive approach, we identify potential risks and implement strategies to prevent adverse events. As a nursing student, I was taught the importance of error prevention, such as medication reconciliation, verification of patient identity, and effective communication with the healthcare team. By adopting evidence-based practices and remaining vigilant in our care, we create a safety culture and ensure our patients’ well-being. As a nurse, always remember that safety is the number one priority, always. Nurses can have their licenses revoked if they are found to practice recklessly. Nurses also need to practice within their scope of practice to remain protected.
For example, a registered nurse can assess and monitor the effects of a medication taken by the patient but cannot change the medication or its dose. I recall caring for a patient after recovering from surgery, but upon my assessment, she could not feel sensations in her legs completely. I immediately placed the patient on fall precautions based on hospital protocols and continued frequent assessments until the effects of anesthesia she previously received were resolved. During this time, she could not get out of bed to prevent a possible fall. The priority was to maintain patient safety and ensure that the time was right based on assessment findings when it was safe for the patient to get out of bed with assistance.
Conclusions
Nursing fundamentals provide the foundation for your nursing education and future practice. Understanding and mastering these key components equips you with the necessary tools to deliver safe, competent, and compassionate care. As you progress on your nursing journey, remember that these fundamental principles will guide you through complex healthcare scenarios, instilling confidence and positively impacting your patients’ lives. Embrace the opportunities to learn, grow, and embody the essence of nursing professionalism, and always prioritize the well-being and safety of those entrusted to your care.
Finally, I encourage nursing students and nurses to continue developing their knowledge, skills, and attitudes to become competent, compassionate nurses who provide high-quality care to their patients. By understanding these 11 key components, you will have a solid nursing career foundation.